Medical Cannabis Course
This course is designed to give you useful background information on medical cannabis, as well as help align your expectations when it comes to seeking access to treatment.
A useful guide to help you get to grips how medical cannabis relates to the body, and its related conditions.
What is Medical Cannabis?
Medical Cannabis
Medical cannabis is a broad term used to refer to any medical products derived from, or related to, cannabis. In legal terminology and the medical field they are often referred to as cannabis-based medicinal products (CBMPs). CBMPs were legalised for use on prescription in November 2018.
There are a number of products that fall into this category, including whole cannabis flower – which can be vaporised, as well as capsules, oils, sprays, and pastilles containing cannabinoids. The main compounds utilised in medical cannabis products are the cannabinoids cannabidiol (CBD) and tetrahydrocannabinol (THC) which have been investigated for their useful therapeutic properties. In addition to cannabinoids, whole cannabis flower or full spectrum extracts of the plant may contain other compounds called terpenes and flavonoids. These compounds are found across all plants and are often responsible for the smell, taste and colour of different plants. There is some research into potential medical properties of these compounds, however this is still an area of growing research.
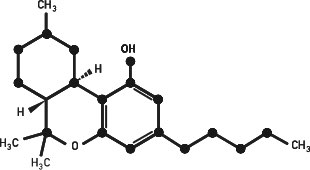
Tetrahydrocannabinol (THC)
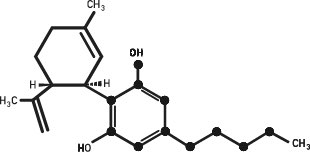
Cannabidiol (CBD)
Currently, Sativex, Nabilone, and Epidyolex are currently the only licensed medical cannabis products in the UK. However, other unlicensed products may also be prescribed in patients where first-line therapies have been unsuccessful.
CBMPs are different from CBD oil available over the counter as all CBMPs are produced to EU Good Manufacturing Practices which ensures consistency in supply and quality. In contrast, CBD oil available on the high street is classified as a novel food and therefore does not have to meet the same stringent regulations regarding its manufacture.
Cannabinoids, THC and CBD
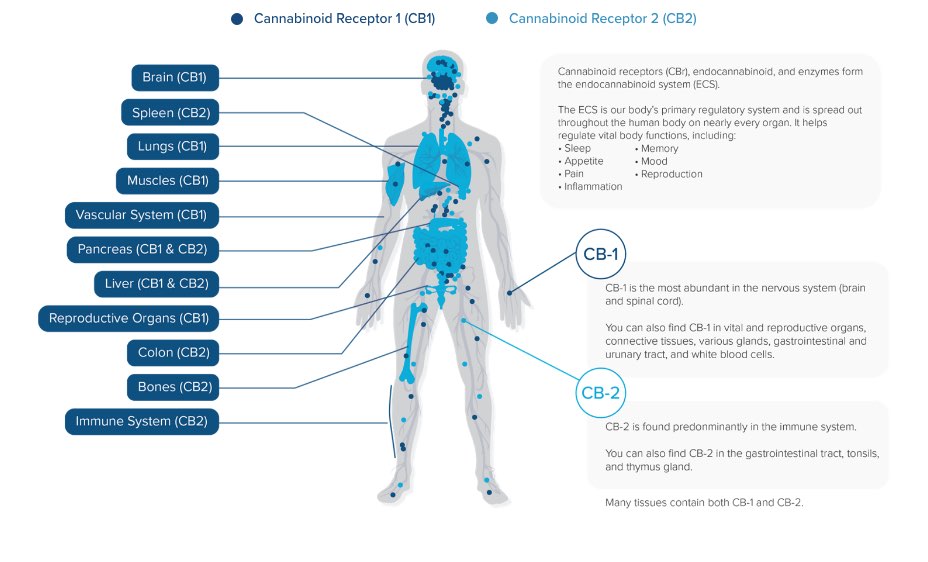
Cannabinoids are compounds that are able to interact with the receptors found in the body’s endocannabinoid system (ECS). The ECS is made up of numerous receptors, cannabinoids and enzymes. The most well studied receptors are known as cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2). CB1 is predominantly found in the brain and is acted upon by the body’s own cannabinoids (endocannabinoids) to regulate emotions, motor coordination and cognition. CB2 is predominantly found in immune cells and activation by endocannabinoids is thought to effect the immune system.
There are over 120 cannabinoids found in the Cannabis plant, the most common being THC and CBD. THC is similar to the endocannabinoids, by having stimulating effects at the CB1 and CB2 receptors. At sufficient doses THC can overstimulate CB1 receptors in the brain resulting in the ‘high’ typically associated with its recreational use. At low doses however, this is not typically experienced.
CBD on the other hand has a diverse role in the ECS. CBD’s main role is thought to be not through direct action at CB1 or CB2 receptors but by inhibiting an enzyme called fatty acid amide hydrolase (FAAH). This enzyme breaks down the body’s main endocannabinoids. By stopping this enzyme from working as it otherwise would it increases the amount of endocannabinoids available to stimulate cannabinoid receptors. However, CBD also works to change the shape of cannabinoid receptors reducing the effects of THC and endocannabinoids. This is thought to be the mechanism by which CBD can alter the effects THC, particularly reducing any associated euphoria or ‘high’.
In addition to their effects on the endocannabinoid system they have indirect and direct effects on receptors that are involved in pain pathways, mood and anxiety levels, inflammation, and movement.
What is the Endocannabinoid System (ECS)?
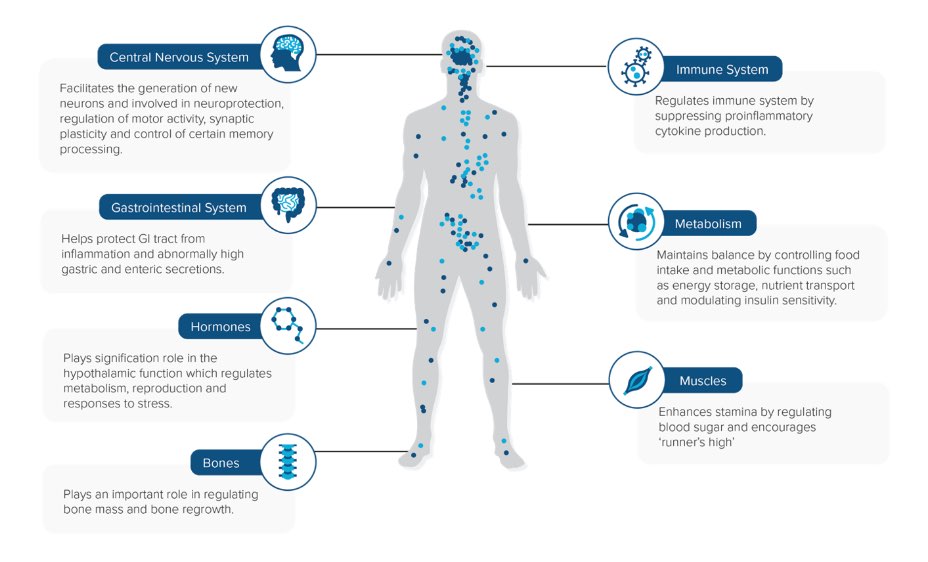
The Endocannabinoid system (ECS)
The endocannabinoid system (ECS) is a neuro-modulatory system expressed throughout the human central nervous system and the immune system. The ECS consists of neurotransmitters (known as endocannabinoids), receptors, and enzymes. Both endocannabinoids as well as cannabinoids derived from cannabis (phytocannabinoids) are able to interact with these receptors (CB1 and CB2). The endocannabinoid system has been found to play a role in a number physiological and cognitive functions including the regulation of mood, memory, appetite, temperature, and hormone levels as well pain signalling and inflammation. Which Conditions can Medical Cannabis be Prescribed for?
Medical cannabis may be prescribed in a number of conditions
Medical cannabis products can currently be considered for use for a number of indications and can be prescribed by a specialist clinician, supported by a multi-disciplinary team, for diagnosed conditions where first-line therapies have failed. GPs can only prescribe medical cannabis under a shared care agreement with a specialist doctor. GPs can refuse to prescribe medical cannabis products if they believe that they do not have the necessary knowledge to do so.
Pain Conditions
- Chronic pain
- Fibromyalgia
- Migraine
- Cluster Headache
- Neuropathic pain
- Cancer-Related Pain
- Ehlers Danlos Syndromes
- Palliative Care
Psychiatric Conditions
- ADHD
- Anxiety
- Agoraphobia
- Autistic Spectrum Disorder
- Depression
- Insomnia
- OCD
- PTSD
- Tourette’s Syndrome
Neurological Conditions
- Autistic Spectrum Disorder
- Epilepsy
- Migraine
- Cluster headache
- Multiple Sclerosis
- Neuropathic pain
- Parkinson’s Disease
Gastrointestinal
- Crohn’s Disease
- Ulcerative Colitis
- Irritable Bowel Syndrome (IBS)
Cancer Related Conditions
- Anxiety
- Nausea and Vomiting
- Appetite Loss
- Depression
- Palliative Care
Contraindications
Medical cannabis products are currently not recommended for use in patients who are/have:
- Pregnancy/breast feeding
- Ongoing or active psychosis
- Unstable cardiovascular disease
- Allergic reactions to ingredients or excipients
Caution
When prescribing medical cannabis, health professionals should be cautious of:
- Children/adolescents
- Interacting medicines
What is the Evidence on Medical Cannabis?
General Evidence for Medical Cannabis
Humans have been using cannabis for a number of indications for thousands of years, however, our scientific understanding of the active compounds within the plant has only developed in recent decades. Due to the interactions between cannabinoids and the human endocannabinoid system, medical cannabis may be prescribed for a large number of indications.
According to the UK Medical Cannabis Registry, chronic pain is the most common reason why people are prescribed medical cannabis. After this the next most common are psychiatric and neurological conditions.
Clinical research into medical cannabis is still in its infancy so there remains a general lack of high-quality clinical evidence to either support, or oppose, the use of CBMPs. However, there is a large base of real world evidence, such as that collected in databases and registries.
Common Side Effects
The side effects of medical cannabis can vary widely depending on the patient and the products used. The existing evidence suggests that side effects can differ from mild to serious and can include:
Very common side effects (more than one in 10 people)
- feeling drowsy or sleepy
- decreased appetite
- diarrhoea
- fever
- feeling tired
- vomiting or nausea
Common side effects (more than 1 in 100 people)
- lack of energy or giddy
- blurred vision
- eating more than usual
- difficulty speaking
- change of taste or dry mouth
- constipation/diarrhoea
- cold, sore throat/mouth
- respiratory tract infections (pneumonia, bronchitis)
- blood tests showing increases in levels of certain liver enzymes or damage to the liver (signs include: abdominal pain, unexplained nausea and malaise, darkening of urine or jaundice)
- shaking, of the body or parts of it
- feeling bad-tempered (irritable, aggressive)
- difficulty sleeping
- cough
- rash
- increased appetite or weight loss
- sialorrhea (drooling)
- urinary tract infection
- abnormal behaviours or agitation
- loss of balance or falling over
Uncommon (affecting less than 1 in 100 people)
- fainting
- changes in pulse rate, heart rate or blood pressure
- tummy pain
- mouth or teeth changing colour